Industry
Highlights
- Healthcare organizations still use traditional mediums to drive patient care coordination.
- Data interoperability has become integral to the healthcare industry as it shifts from a provider-centered model to a patient-centered one.
- The right open data exchange platform can enable seamless data exchange with ecosystem partners, aggregate and analyze data to predict health risk events, and alert, notify, or nudge the patient treating team for prompt action.
On this page
Realizing the full potential of interoperability
The healthcare industry has shifted focus from a provider-centered model to a patient-centered one.
The latter empowers, engages, and activates the patients in their healthcare journey, and data interoperability becomes the single most critical element to drive this shift. The most prominent challenges that healthcare providers face while implementing true interoperability and solving the healthcare fragmentation problem are:
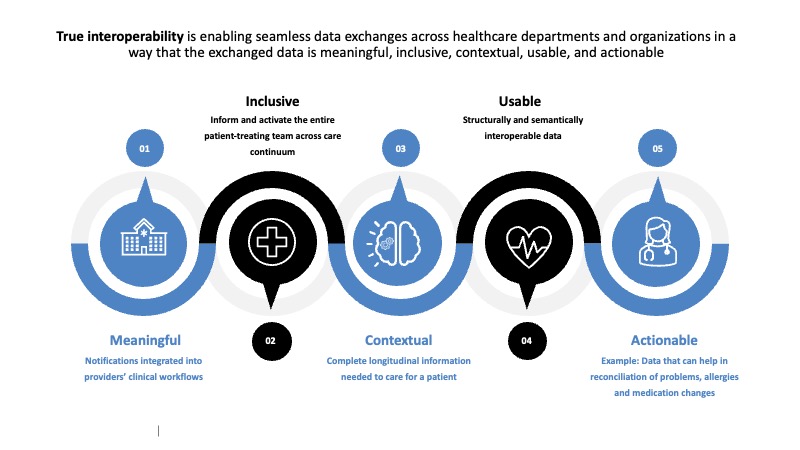
- Enabling seamless data exchanges across healthcare departments and organizations in a way that the exchanged data is meaningful, inclusive, contextual, usable, and actionable
- Creating and preserving a consistent clinical document approach
- Steering provider adoption
Navigating the expectations and barriers
Most healthcare organizations still use faxes and secure emails to drive patient care coordination.
This is despite electronic health record (EHR) adoption being above 95% in US hospitals and 80%-90% for office-based physicians. Implementing secure direct notification integrated into the workflow of providers involved in patient care is still challenging across disparate EHRs.
Patient-treating teams are not entirely in sync and hence, not fully activated. All healthcare providers of a patient must be in the know as to when that patient goes to an emergency department, gets admitted, or is discharged from a hospital. Admission, discharge, and transfer (ADT)-based secure direct notifications should help providers contact the patient early, reinforcing the treatment plan upon getting discharged, arranging for a very early follow-up with a chronic disease specialist, and, perhaps, finding a primary care physician (PCP) if one does not already exist. Through meaningful granular payloads, ADT-based secure direct notification should ensure seamless and timely communication between disparate systems across disparate care locations (acute care, home care, ambulatory care, among others) and healthcare payers. Such payloads should communicate much more than just letting the primary care physician know when a patient was admitted or discharged.
For patients with multiple medical conditions and those who visit multiple specialists, it is crucial to have all the participating providers, patient treating teams, and payers are on the same page. Any changes to the patient’s treatment plan ought to be easily and meaningfully communicated to all stakeholders, in an inclusive manner. Handling proper identification of the post-acute and outpatient care teams, including primary care physician, patient privacy, and any security issues, is critical to engaging and activating the entire patient-treating team.
Patient-centric open data exchange platform
Patients with one or more chronic conditions receive care across an ever-widening array of facilities (hospitals, homes, clinics, urgent care, imaging centers, and the like).
This underscores the need for a patient-centric open data exchange interoperability platform. Many facilities are not fully equipped to view and track patient care across different healthcare settings.
The vast volumes and types of healthcare data and the fast-growing adoption of digital health technologies (telehealth or mobile health applications, wearable devices, remote monitoring solutions) accentuate the need for healthcare systems to transform into secure open data exchanges to consume and share interoperable data with the ecosystem. True interoperability means that as patients move across healthcare settings, their data follows them, and patient-centric open data exchange platforms should enable the same.
The 21st Century Cures Act allows patients unrestricted digital access to complete health records. With appropriate patient consent workflows, the open data exchange platform can consume this patient data, enable seamless data exchange with ecosystem partners, aggregate and analyze data to predict health risk events, and alert, notify, or nudge the patient treating team promptly for intervention.
Fast Healthcare Interoperability Resources (FHIR) enable the integration of push-based data exchange with pull-based data access. The pull-based model makes the data access more patient-centric with less investment by identifying the entire patient-treating team and then sharing the data with them. The model makes the data available for immediate consumption using APIs. Simply put, the consumers (care delivery or management teams) can pull patient-related data from the open data exchange using FHIR APIs on demand and in real time. In this model, the consumers also become the producers of interoperable data and play both roles in delivering seamless and meaningful data exchange.
FHIR API-based open data exchange platform enables two primary capabilities to implement patient-centric care:
- Clinical integration with hospitals and provider communities by creating a single interoperable longitudinal patient record from clinical, financial, administrative, self-reported patient data and other data from disparate information systems or sources and of different data types
- Point solutions using smart apps that can be developed and integrated seamlessly
An integrated clinical experience
The clinical integration channel consumes and shares information about all the care a patient has received seamlessly using FHIR APIs.
This helps provide an integrated clinical experience for all payers and providers participating in patient care. This data exchange platform includes electronic medical record (EMR) or electronic health record (EHR) connectors (that can be used to connect to any hospital system that shares EMR or EHR data using FHIR APIs), FHIR data mapper (that accelerates mapping non-FHIR data into FHIR resources), and other FHIR-enabling accelerators, including the validators. These components can connect to and consume data from various sources, including EMR or EHR systems, health data systems, wearable devices (patient-shared data), software as a service (SaaS) applications, and other services.
The data consumed is exposed through RESTful APIs using a FHIR server platform. The APIs can be accessed by patients and participating providers (doctors, nurses, and other caregivers) and payer systems across the care continuum to visualize a comprehensive and curated picture of a unified longitudinal view of patient care and health data, connect and collaborate to improve patient’s connected care experience and health outcomes, and control the cost of care. Some practical use cases where providers and payers can leverage comprehensive and curated picture include:
- Identifying and closing care gaps
- Identifying clinically unnecessary or duplicate care or diagnostic tests
- Identifying conflicting care plans
- Identifying potential adverse prescription drug interactions
- Removing redundant costs associated with all such identified problems
- Activating and involving the patient in the clinical programs
Get smart with point solutions
Point solutions can be visualized as built-for-purpose solutions within the workflows of healthcare payer and provider systems.
The open data exchange powered by FHIR can be leveraged to rapidly build Substitutable Medical Applications and Reusable Technologies (SMART)-on-FHIR apps. Such built-for-purpose apps, supporting patients, providers, employers, other payers, and entities, can rapidly deliver value to improve operational efficiencies, patient engagement and empowerment, and targeted care management for specific conditions.
Some practical use cases for SMART-apps-based point solutions would include:
- Condition management – Combining clinical and claims data to handle weight and nutrition information and to support other lifestyle changes.
- Administrative simplification – Payers typically access a provider portal for providers to check member eligibility and claim status. This can be integrated with FHIR-based SMART apps to rapidly access and understand coverages or eligibility data, and claim status data, thereby reducing inbound calls and enabling interoperability between administrative and clinical systems.
- Smart platform for patients – The patient-centric data exchange interoperability platform aggregates patient data from all the connected facilities and presents them through FHIR-based APIs. Patients will be given access to this unified and comprehensive information via the smart app, which aims to involve, enable, and activate the patient in their care and clinical programs.
Clinical integration drives collaborative care delivery and holistic health provision for members. The model also enables real-time interoperable interfaces between providers, payers, employers, regulatory bodies, and other ecosystem partners, as well as member apps that can talk to each other with less time, money, and resources spent on integration-related efforts.